It’s safe to say today’s marijuana is not like the marijuana of even a few decades ago. Levels of tetrahydrocannabinol, or THC, the psychoactive component in cannabis responsible for producing a high, used to average around 2% in the 1960s. Today, that number often exceeds 20%, and some extracts can even exceed 90%.
Now legalized for adult recreational and medicinal use in 10 states and the District of Columbia, the public perception of cannabis continues to shift towards greater acceptance despite significant research pointing to the harmful role the drug could be playing in the public health arena, not least of which is a relationship between marijuana and psychosis.
We talked to Dr. Jan A. Mayer, a Nashville-based psychiatrist and expert on addiction, about some of the latest findings on marijuana and psychosis and what you need to know if you or someone you love is affected by marijuana addiction.
1. There is substantial evidence linking marijuana and incidences of psychosis.
The National Academies of Sciences, Engineering, and Medicine (NASEM) reported in 2017 “substantial evidence of a statistical association between cannabis use and the development of schizophrenia or other psychoses, with the highest risk among the most frequent users.” While probably just about anyone who has ever smoked pot can share a story about feeling paranoid, anxious, or experiencing unpleasant thoughts, what NASEM is reporting is something more severe. One source of evidence of this exists in increased emergency room visits.
The Journal of Adolescent Health reported in 2018 that between 2005 and 2015 marijuana-related illness emergency department and urgent care visits rose by 3.1% in individuals ages 13 to 20 in Colorado where marijuana is legal. One of the lead authors of the study, Dr. George Wang, wrote, “Marijuana-related (emergency department/urgent care) visits are of significant concern as patients are having significant acute medical or psychiatric symptoms requiring evaluation.”
Additionally, of the 1.25 million emergency department visits related to illicit drug use reviewed in a 2011 study by the Substance Abuse and Mental Health Services Administration (SAMSHA) and the Drug Abuse Warning Network (DAWN), nearly 40% involved marijuana.
“The severity and incidence of prevalence is going up because people are getting higher doses of THC,” says Mayer. And the more frequently someone uses, like chronic daily smokers, the higher the risk of experiencing a substance-induced psychotic disorder, also sometimes called cannabis-induced psychosis (CIP).
2. Schizophrenia and substance-induced psychotic disorders are very different.
While studies show a relationship between marijuana and schizophrenia, there hasn’t been definitive evidence that marijuana can cause schizophrenia. It’s a classic medical chicken-egg scenario: does using marijuana cause schizophrenia or does someone with schizophrenia use marijuana in an attempt to self-medicate?
What the research does indicate though is that marijuana could trigger a schizophrenic episode, especially in individuals genetically predisposed to the mental illness.
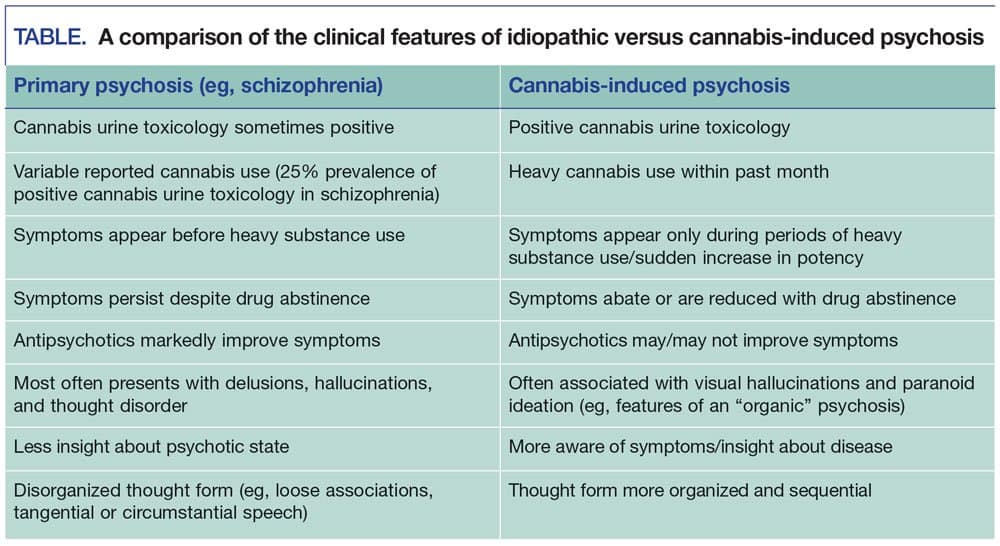
But schizophrenia and CIP are very different types of psychosis. Mayer points out that one of the primary ways to tell the difference between the two is that with CIP, psychotic symptoms will diminish or disappear when the substance isn’t used.
It can get tricky, however, especially if someone is a marijuana addict and does not maintain periods of abstinence.
“Marijuana is probably the hardest thing to treat,” says Mayer. “When people stop using marijuana they get withdrawal but they don’t recognize it as withdrawal. They think marijuana was helping them with anxiety and sleep, and when they stop they have this very uncomfortable anxiety, insomnia, irritability, depression. So, they think marijuana was keeping them from having that to start with, which it doesn’t by the way—it causes .
Other hallmarks of CIP are visual hallucinations and paranoid ideation rather than the more delusional thinking and thought disorder found with schizophrenia. More simply, someone with schizophrenia will not have the insight to know he is having a psychotic episode.
With schizophrenia, prescription antipsychotics will dramatically improve the person’s condition of mind. Because CIP is tied to marijuana use rather than a neurological abnormality, antipsychotics may or may not do anything.
3. It is vital to establish a thorough health history.
It is not uncommon for individuals in early recovery to experience a co-occurring disorder, like a substance use disorder and anxiety or a substance use disorder and depression. In fact, Mayer says, that number can hover around 100%. But with time and recovery in place, many of those co-occurring disorders will slip away in the absence of the offending substance.
It’s vital, however, to get a clear health history in order to provide the best course of treatment. So, in determining the difference between schizophrenia and CIP, it is important to know what some of the symptoms were preceding a psychotic episode. If psychotic symptoms only appear during periods of heavy marijuana use or with very potent cannabis strains, all signs point to CIP. If the psychotic symptoms are present before someone uses or in the absence of cannabis, it could be schizophrenia or some other kind of psychosis.
Obtaining a family health history can also provide a medical provider with a lot of insight as illnesses like schizophrenia have stronger genetic associations than CIP.
4. Adolescents and young adults are at a greater risk for developing a psychotic mental illness from marijuana use.

It’s another area where the research is still being developed, but evidence seems to indicate that adolescents and young adults who use cannabis are at a greater risk for developing a psychotic mental illness. This age group in particular also has access to a greater variety of THC products, like oils and edibles, than previous generations.
The brain is still undergoing neurological development until about the age of 25. The introduction of THC during this time can impede proper development, resulting in a host of issues ranging from depression to a lower IQ. Most psychotic disorders, like schizophrenia, develop in the teen and young adult years.
Like with adults, however, it can be hard to determine if cannabis triggers psychosis, or if an adolescent predisposed to psychosis will use cannabis in an attempt to soothe distressing thoughts and feelings.
5. The best way to prevent cannabis-induced psychosis is to abstain from marijuana.
“If you’ve got somebody that’s a heavy addictive user and they get a marijuana psychosis,” says Mayer, “then they’re at high risk to get it again.” So, the best way to prevent CIP is to abstain from using marijuana.
If quitting feels like an impossible task for you or a loved one, we can help. Contact us to learn more about our 30-Day Residential Program and Long-Term Recovery Program. And be sure to read Tanner’s story, a Discovery Place alum who found freedom from marijuana addiction.

